abbreviations
- IWGDF: International Working Group on the Diabetic Foot
- LOPS: Loss of Protective Sensation
- PAD: Peripheral Arterial Disease
- VPT: Vibration Perception Threshold
- DSPN: Distal Symmetric Polyneuropathy
- ABI: Ankle-Brachial Index
- DM: Diabetes Mellitus
- DFU: Diabetic Foot Ulcer
- TCC: Total Contact Cast
- SPPB: Short Physical Performance Battery
- TCPO2: Transcutaneous Oxygen Tension
- HRQOL: Health-Related Quality of Life
Identifying The Person With An At-Risk Foot
| Risk category | Definition |
| 0 (Very Low Risk) | No LOPS, no PAD, no deformity |
| 1 (Low Risk) | LOPS or PAD |
| 2 (Moderate Risk) | LOPS + PAD, or LOPS + foot deformity or PAD + foot deformity |
| 3 (High Risk) | LOPS or PAD, and one or more of the following:
|
LOPS: loss of protective sensation; PAD: peripheral arterial disease.
Assessment for loss of protective sensation:
10 g monofilament and any one of the following:
- Vibration using a 128-Hz tuning fork
- Biothesiometer (Vibration Perception Threshold (VPT))
- Pinprick sensation
- Ankle reflexes
Evaluation of peripheral artery disease
Vascular status: in case of absent foot pulses or other signs of PAD, consider performing pedal Doppler waveforms in combination with measurement of the ankle pressure & ankle-brachial index and toe pressure & toe-brachial index
Regularly Inspecting And Examining The Person With An At-Risk Foot (IWGDF Risk 1 Or Higher)
| Risk category | Suggested follow-up |
| 0 | Annually (by generalist and/or specialist) |
| 1 | Every 6 to 12 months |
| 2 | Every 3 to 6 months |
| 3 | Every 1 to 3 months (by specialist) |
Regular Inspecting And Examining checklist:
History
| Right | Left | |
| Intermittent Claudication | ||
| End Stage Renal Disease | ||
| Foot Ulcer | ||
| History of Foot Ulceration | ||
| History of Foot amputation | ||
| DSPN Symptoms |
Examination
| Right | Left | |
| Footwear |
| Right | Left | |
|
Skin Color |
|
|
|
Oedema |
|
|
|
Tinea Pedis |
|
|
|
Hairless Skin |
|
|
|
Foot Fissure |
|
|
|
Foot Dryness |
|
|
|
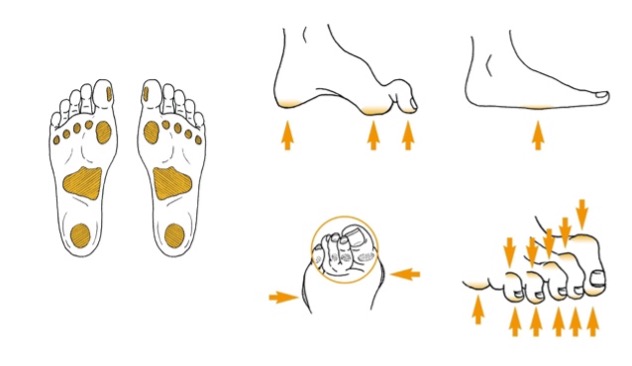
Callus |
|
|
|
Foot Hemorrhage |
|
|
|
Thick Or Ingrowing Tonail |
|
|
| Cut Toenails
|
||
| Unwashed Feet
|
| Right | Left | |
|
10 Gram Monofilament |
||
|
Vibration Perception |
||
|
Lightly Touch |
| Right | Left | |
|
Posterior Tibial Pulses |
||
|
Dorsalis Pedis |
||
|
ABI |
| Right | Left | |
|
Claw Toes |
||
|
Hammer Toes |
||
|
Large Bony Prominences |
||
|
Limited Joint Mobility |
||
|
Flat Foot |
Education On Foot Self-Care (IWGDF Risk 1 Or Higher)
- Avoid going barefoot, even at home, and especially on hot decks and hot sand or any activity may injure or cause burn for foot.
- Test water temperature before stepping into a bath
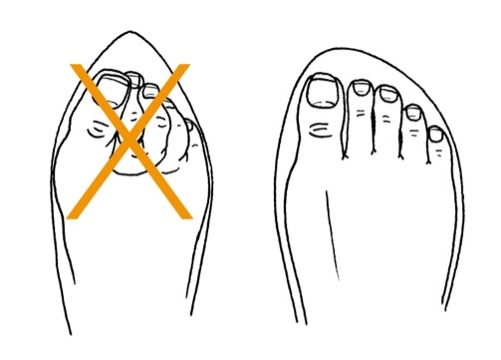
- Trim toenails straight to shape of the toe, and remove sharp edges with a nail file; do not cut cuticles
- Wash in lukewarm water, dry thoroughly (including between the toes), and check feet daily
- Shoes should be snug, but not tight, and customized if feet are misshapen or there is a history of ulcers
- Select shoes that are snug but not tight, with a wide toe box, and break new shoes in gradually to prevent any blisters.
- Check that there is nothing in your shoes before wearing them.
- Wear cotton socks that fit well, and be sure to change your socks every day.
- Check daily the entire surface of both feet for skin breaks, blisters, swelling, or redness, including between and underneath the toes where damage may not be easily visible.
- Seeking professional help in a timely manner after identifying a foot problem
- Avoid smoking
- Go for a yearly Diabetic Foot Screening at a polyclinic, GP clinic, or hospital.
Instructions About Foot Self-Management (IWGDF Risk 1-3)
Consider coaching a person with diabetes who is at moderate or high risk of foot ulceration (IWGDF risk 2-3) to self-monitor foot skin temperatures once per day to identify any early signs of foot inflammation and help prevent a first or recurrent plantar foot ulcer. Encourage Routine Wearing Of Appropriate Footwear (IWGDF risk 1-3) In persons with diabetes and IWGDF risk category 1 or higher, wearing inappropriate footwear or walking barefoot are major causes of foot trauma leading to foot ulceration.
Appropriate Footwear :
- The inside length of the shoe should be 1-2 cm longer than the foot and should not be either too tight or too loose
- The internal width should equal the width of the foot at the metatarsal phalangeal joints (or the widest part of the foot)
- And the height should allow enough room for all the toes.
- Evaluate the fit with the patient in the standing position, preferably later in the day (when they may have foot swelling).
- If there is no off-the-shelf footwear that can accommodate the foot (e.g., if the fit is poor due to foot deformity) or if there are signs of abnormal loading of the foot (e.g., hyperaemia, callus, (previous) ulceration), prescribe therapeutic footwear, possibly including extra-depth shoes, custom-made footwear and custom-made insoles. This may also include the prescription and fabrication of (toe) orthoses.
Footwear should be sufficiently wide to accommodate the foot without excessive pressure on the skin
Treating risk factors for ulceration and pre-ulcerative signs in persons with IWGDF risk 1-3
- Provide appropriate treatment of excess callus on the foot, for ingrown toe nails, and for fungal infections on the foot.
- Treat any (modifiable) pre-ulcerative sign on the foot including protecting blisters, or draining them if necessary.
- Consider coaching a person with diabetes who is at moderate or high risk of foot ulceration (IWGDF risk 2-3) to self-monitor foot skin temperatures once per day to identify any early signs of foot inflammation and help prevent a foot ulcer.
- When excess callus or a pre-ulcerative lesion is present on the apex or distal part of a non-rigid hammertoe, consider digital flexor tendon tenotomy or consider prescribing orthotic interventions.
- The risk for foot ulceration is not a barrier to participating in a physical training program as long as appropriate footwear is worn, with a gradual increase in activity to an additional 1000 steps/day. In addition, a foot-ankle exercise program may be considered.
Foot-related exercises and weight-bearing activity
- Consider advising and referring a person with diabetes who is at low or moderate risk for foot ulceration (IWGDF risk 1 or 2) to participate in an 8-12-weeks foot-ankle exercise program, preferably under the supervision of an appropriately trained healthcare professional, and to continue performing foot-ankle exercises afterwards, with the aim of reducing risk factors of ulceration.
- Consider communicating to a person with diabetes who is at low or moderate risk for foot ulceration (IWGDF risk 1 or 2) that an increase in the level of walking-related weightbearing daily activity by an extra 1000 steps/day is likely to be safe regarding risk of foot ulceration. Advise this person to wear appropriate footwear when undertaking weight-bearing activities, and to frequently monitor the skin for (pre-)ulcerative lesions.
