Abbreviations
- DM: Diabetes Mellitus
- PAD: Peripheral Arterial Disease
- LOPS: Loss of Protective Sensation
- ABI: Ankle-Brachial Index
- UKST: United Kingdom Screening Test
- VPT: Vibration Perception Threshold
- SINBAD: Site, Ischemia, Neuropathy, Bacterial infection, Area, and Depth
- IWGDF: International Working Group on the Diabetic Foot
- IDSA: Infectious Diseases Society of America
- WIfI: Wound, Ischemia, and foot Infection
- TcPO2: Transcutaneous Oxygen Tension
- SIRS: Systemic Inflammatory Response Syndrome
- ESR: Erythrocyte Sedimentation Rate
- CRP: C-Reactive Protein
- CBC: Complete Blood Count
- MR: Magnetic Resonance
- HBOT: Hyperbaric Oxygen Therapy
- NPWT: Negative Pressure Wound Therapy
- DFU: Diabetic Foot Ulcer
- MRI: Magnetic Resonance Imaging
- HbA1c: Hemoglobin A1c
- PET: Positron Emission Tomography
- TMA: Transmetatarsal Amputation
- DM: Diabetes Mellitus (repeated for context)
INTRODUCTION
Diabetic foot refers to a variety of foot problems that occur in individuals with diabetes due to complications such as neuropathy, peripheral arterial disease (PAD). These complications can lead to a higher risk of ulcers, infections, and in severe cases, amputations.
The lifetime risk of a foot ulcer for patients with type 1 or 2 diabetes may be as high as 34 percent.
APPROACH
History
Pertinent history to obtain includes :
- Duration of diabetes
- Overall glycemic management
- Presence of micro- or macrovascular disease
- History of prior foot injury resulting in deformities or prior ulcers
- Lower limb vascular bypasses or amputation
- Presence of claudication
- History of cigarette smoking.
- Systemic inflammatory response (malaise, anorexia, fever or chills)
- Collect symptoms of diabetic neuropathy using (UKST).
Foot Examination
General Appearance and Vital Signs:
- High temperature, increased heart rate, or increased respiratory rate.
Inspection –
Dermatologic:
Skin status:
- Color
- Thickness
- Dryness
- Cracking Sweating
Infection:
- Swelling
- Induration
- Erythema
- Tenderness or pain
- Warmth
- Purulent discharge
- Check between toes for fungal infection
Ulceration:
- Calluses/blistering – hemorrhage into callus?
Musculoskeletal:
- Deformity (e.g., claw toes, prominent metatarsal heads, Charcot joint, bunions)
- Muscle wasting (guttering between metatarsals)
Neurologic Assessment:
- 10 g monofilament + 1 of the following 4:
- Vibration using 128 Hz tuning fork
- Pinprick sensation
- Ankle reflexes
- Vibration Perception Threshold (VPT)
Vascular Assessment:
- Foot pulses
- Ankle-Brachial Index (ABI), if indicated
VPT: vibration-perception threshold; ABI: ankle brachial index.
ASSESSMENT OF FOOT ULCERS
Ulcer Classification
- Ulcer can be classified according to the SINBAD system.
- Infection severity should be classified according to the IWGDF/IDSA system.
- Ischemia as part of the WIfI system.
Ulcer Type
- Neuropathic (LOPS, but no PAD)
- Neuro-ischemic (LOPS and PAD)
- Ischemic (PAD, but no LOPS).
|
Ulcer Types |
||
|
Characteristics |
Neuropathic foot |
Neuro ischemic foot |
|
Skin temperature |
Warm |
Cold |
|
Pain |
Painless |
Painful |
|
Skin colour |
Not altered |
Dependent red |
|
Callus |
Thick at pressure points |
Usually not present |
|
Ulcer |
Usually on tips of toes and planter surfaces under metatarsal heads. |
On margins of foot ,tips of toes ,heels. |
|
Peripheral pulses |
Bounding |
Absent |
|
ABI |
More than 0.9 |
Less than 0.9 |
|
Complications |
Charcot Joints |
Critical ischemia |
Classification of the foot ulcer SINBAD Scoring System
SINBAD uses a scoring system with a maximum of 6 points. A score of 3 or more is associated with an increased time to healing and greater risk of eventual failure to heal.
|
SINBAD scoring system |
||
|
Site |
Forefoot |
(0 points) |
|
Midfoot and hindfoot |
(1 point) |
|
|
Ischemia* |
Pedal blood flow intact: at least one palpable pulse. |
(0 points) |
|
Clinical evidence of reduced pedal flow. |
(1 point) |
|
|
Bacterial infection** |
None |
(0 points) |
|
Present |
(1 point) |
|
|
Neuropathy |
Protective sensation intact. |
(0 points) |
|
Protective sensation lost |
(1 point) |
|
|
Area |
Ulcer <1 cm² |
(0 points) |
|
Ulcer ≥1 cm² |
(1 point) |
|
|
Depth |
Ulcer confined to skin and subcutaneous tissue |
(0 points) |
|
Ulcer reaching muscle, tendon, or deeper |
(1 point) |
|
|
Total Score: 0 – 6 |
||
* Assess Ischemia: if pedal blood flow is intact (at least one palpable pulse),
or if there is clinical evidence of reduced blood flow
Consider:
Arterial pedal wave forms (with a Doppler instrument).
Measure the ankle and toe pressures, and calculate the ankle-brachial index (ABI) and toe-brachial index (TBI).
PAD is less likely in the presence of triphasic or biphasic pedal Doppler waveforms, an ABI 0.9-1.3, and a TBI ≥0.70. In selected cases, transcutaneous pressure of oxygen (TcpO2) can be useful.
IWGDF/ Infectious Diseases Society of America (IDSA) system
Classify and document the severity of any infection as mild, moderate or severe using the IWGDF/ IDSA system
|
Infection severity |
Clinical manifestations of infection |
|
(1) Uninfected |
Wound lacking purulence or any manifestations of inflammation |
|
(2) Mild |
Presence of ≥2 manifestations of inflammation (purulence, or erythema, pain, tenderness, warmth, or induration), but any cellulitis/erythema extends ≤2 cm around the ulcer, and infection is limited to the skin or superficial subcutaneous tissues; no other local complications or systemic illness. |
|
(3) Moderate |
Infection (as above) in a patient who is systemically well and metabolically stable but which has ≥1 of the following characteristics: cellulitis extending >2 cm, lymphangitic streaking, spread beneath the superficial fascia, deep-tissue abscess, gangrene, and involvement of muscle, tendon, joint or bone. |
|
(4) Severe |
Infection in a patient with systemic toxicity or metabolic instability (eg, fever, chills, tachycardia, hypotension, confusion, vomiting, leukocytosis, acidosis, severe hyperglycemia, or azotemia). |
Foot ischemia may increase the severity of any infection, and the presence of critical ischemia often makes the infection severe.
NICE (in UK) Guideline System For Classify Severity of Infection
Classify and document the severity of any infection according to the NICE (in UK) guideline system
|
Infection severity |
Clinical manifestations of infection |
|
Uninfected |
Wound lacking purulence or any manifestations of inflammation. |
|
Mild |
presence of ≥2 of local swelling or induration, erythema, local tenderness or pain, local warmth, or purulent discharge, but infection involves only the skin and subcutaneous tissue. If erythema, must be 0.5 cm to <2 cm around the ulcer (exclude other causes of inflammatory response, such as trauma, gout, acute Charcot neuro-osteoarthropathy, fracture, thrombosis, and venous stasis). |
|
Moderate |
local infection with erythema >2 cm around the ulcer or involving structures deeper than skin and subcutaneous tissues (such as abscess, osteomyelitis, septic arthritis, or fasciitis), and no systemic inflammatory response signs.[ |
|
Severe |
local infection with signs of systemic inflammatory response (such as temperature of >38°C [>100.4°F] or <36°C [<96.8°F], increased heart rate, or increased respiratory rate). |
Diagnose infection by the presence of at least two clinical signs or symptoms of inflammation (redness, warmth, induration, pain/tenderness) or purulent secretions.
Abscess and Osteomyelitis need further investigations like: plain X-ray; high levels of ESR, CRP, or procalcitonin or MRI.
For clinically infected wounds obtain a tissue specimen for culture (and Gram-stained smear, if available) by curettage or biopsy, avoid using a swab; consider bone biopsy in case of osteomyelitis.
The causative pathogens (and their antibiotic susceptibilities) vary by geographic, demographic and clinical situations, but Staphylococcus aureus (alone, or with other organisms) is the predominant pathogen in most cases of superficial infections. Chronic and more severe infections are often polymicrobial, with aerobic gram-negative rods especially in warmer climates and obligate anaerobes accompanying the gram-positive cocci.
Threatened limb classification: WIfI scoring
In a person with diabetes and a foot ulcer who is being managed in a setting where appropriate expertise in vascular intervention is available, the IWGDF recommends wound, ischemia, and foot infection (WIfI) classification system scoring to aid assessment of perfusion and the likelihood of benefit from revascularization where this is deemed appropriate for the patient.[3]
The Society for Vascular Surgery lower extremity threatened limb classification system: risk stratification based on WIfI.
A simple Venn diagram has been designed to assist clinicians in defining what specific factor is dominant.
Wound (W):
|
|
Severity |
Description |
|
Wound (W): |
0: |
No ulcer or gangrene |
|
1: Mild |
Small, shallow ulcer(s) on distal leg or foot; no exposed bone (unless limited to distal phalanx);no gangrene |
|
|
2: Moderate |
Deeper ulcer with exposed bone, joint, or tendon; generally not involving the heel;shallow heel ulcer without calcaneal involvement; gangrenous changes limited to digits |
|
|
3: Severe |
Extensive, deep ulcer involving forefoot and/or midfoot; deep, full thickness heel ulcer and/or calcaneal involvement; extensive gangrene involving forefoot and/or midfoot; full thickness heel necrosis and/or calcaneal involvement. |
Ischemia (I)
|
Severity |
ABI |
Ankle Systolic Pressure (mmHg) |
TP, TcPO2 (mmHg) |
|
|
Ischemia (I) |
0: |
≥0.80 |
>100 |
≥60 |
|
1: Mild |
0.6 – 0.79 |
70 – 100 |
40 – 59 |
|
|
2: Moderate |
0.4 – 0.59 |
50 – 70 |
30 – 39 |
|
|
3: Severe |
≤ 0.39 |
< 50 |
< 30 |
Foot infection (fI)
|
|
Severity |
Description |
|
Foot infection (fI) |
0: |
No symptoms or signs of infection Infection present, as defined by the presence of at least two of the following:
|
|
1: Mild |
Local infection involving only the skin and the subcutaneous tissue (without involvement of deeper tissues and without systemic signs as described below). | |
|
2: Moderate |
Local infection (as described above) with erythema >2 cm, or involving structures deeper than skin and subcutaneous tissues (e.g., abscess, osteomyelitis, septic arthritis, fasciitis); no systemic inflammatory response signs |
|
|
3: Severe |
Local infection (as described above) with the signs of the systemic inflammatory response syndrome ( SIRS), as manifested by two or more of the following:
|
|
|
Add “(O)” |
Infection involving bone (osteomyelitis) |
ABI: Ankle-Brachial Index; PaCO2 : Partial Pressure of Carbon Dioxide; SIRS: Systemic Inflammatory Response Syndrome; TcPO2 : Transcutaneous Partial Oxygen Pressure; TMA: Transmetatarsal Amputation; TP: Toe Pressure
Wagner’s Classification of diabetic ulcer According to severity;
|
Grade |
Clinical Finding |
|
0 |
Intact skin (impending ulcer) |
|
1 |
Superficial ulcer – Skin and subcutaneous tissue only |
|
2 |
Deep ulcer to tendon, muscle, joint capsule, or bone |
|
3 |
Deep ulcer with abscess, osteomyelitis, or tendinitis |
University of Texas system (UT)
|
Grade |
Clinical Finding |
Stage |
|
0 |
Pre- or postulcerative |
|
|
1 |
Full-thickness ulcer not involving tendon, capsule, or bone |
|
|
2 |
Tendon or capsular involvement without bone palpable |
|
|
3 |
Probes to bone |
INVESTIGATIONS
1st test to order
|
Test |
Comment |
|
CBC , CRP, ESR |
|
|
X-Ray Foot |
Plain radiographs can detect structural foot deformities, soft tissue gas, and foreign bodies and may be able to detect osteomyelitis. |
|
Renal function |
Other tests to consider
|
Test |
Comment |
|
Angiography |
Considered to be the best test for diagnosing peripheral artery disease. |
|
MR angiography |
Can be used to obtain anatomical information when considering revascularizing a patient’s lower extremity. |
|
MRI foot |
Diagnosing osteomyelitis. |
|
Arterial Duplex Ultrasound |
Assessment of the peripheral arterial circulation |
TREATMENT OF A FOOT ULCER
Standard management of diabetic foot ulcers involves one or more of:
Offloading
Control of foot infection
Control of ischemia
Wound debridement
Wound dressings.
Determining the cause of the ulcer
Always try to determine the precipitating event that led to ulceration, this information is relevant both for treatment plans and for prevention of recurrence. Look for abnormal walking patterns, deformities, bony prominences and other foot abnormalities (supine and standing) that could have contributed to ulceration. Wearing ill-fitting shoes and walking barefoot are practices that frequently lead to foot ulceration, even in patients with exclusively ischemic ulcers. Therefore, meticulously examine shoes and footwear behavior in every patient with a foot ulcer as part of cause determination.
Assessment of person-related factors
Apart from a systematic evaluation of the ulcer, the foot and the leg, also consider person-related factors that can affect ulcer healing and affect treatment. These factors include kidney function/end-stage renal disease, oedema, malnutrition, poor metabolic control, depression or other psycho-social problems, and frailty.
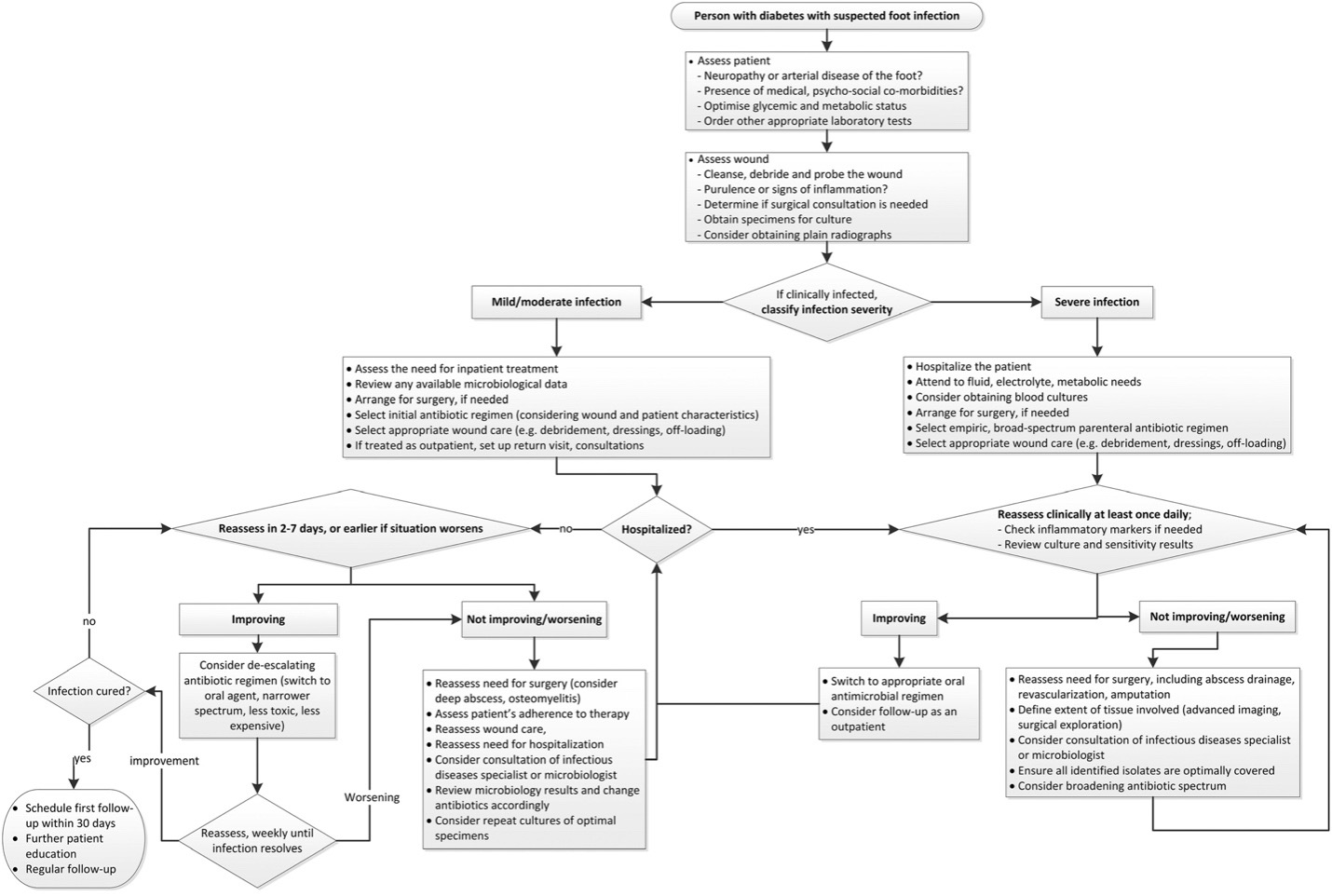
Control of foot infection
- Assess the severity of any diabetes-related foot infection using the IWGDF/IDSA classification scheme.
- Consider a sample for culture to determine the causative microorganisms, preferably by aseptically collecting a tissue specimen (by curettage or biopsy) from the wound.
- Consider hospitalizing all persons with diabetes and a foot infection who have either a severe foot infection as classified by the IWGDF/IDSA classification, or a moderate infection which is associated with key relevant morbidities.
Findings suggesting a more serious diabetes-related foot infection and potential indication for hospitalization:
|
Wound specific |
|
|
Wound |
Penetrates to subcutaneous tissues (e.g., fascia, tendon, muscle, joint, or bone) |
|
Cellulitis |
Extensive (>2 cm), distant from ulceration, or rapidly progressive (including lymphangitis) |
|
Local signs / symptoms |
Severe inflammation or induration, crepitus, bullae, discoloration, necrosis or gangrene, ecchymoses or petechiae, and new anesthesia or localized pain |
|
General |
|
|
Presentation |
Acute onset/worsening or rapidly progressive |
|
Systemic |
Fever, chills, hypotension, confusion, and volume depletion |
|
Laboratory tests |
Leukocytosis highly elevated C-reactive protein, or erythrocyte sedimentation rate, severe or worsening hyperglycemia, acidosis, new/worsening azotaemia and electrolyte abnormalities tests |
|
Complicating features |
Presence of a foreign body (accidentally or surgically implanted), puncture wound, deep abscess, arterial or venous insufficiency, lymphedema, immunosuppressive illness or treatment, acute kidney injury |
|
Failing treatment |
Progression while on apparently appropriate antibiotic and supportive therapy |
Factors that should lead to considering hospitalization
|
Factors that should lead to considering hospitalisation |
|
· Severe infection (see findings suggesting a more serious diabetes-related foot infection above) |
|
· Metabolic or haemodynamic instability |
|
Intravenous therapy needed (and not available/appropriate as an outpatient) |
|
Diagnostic tests needed that are not available as an outpatient |
|
· Severe foot ischaemia is present |
|
· Surgical procedures (more than minor) required |
|
· Failure of outpatient management |
|
· Need for more complex dressing changes than patient/caregivers can provide |
|
· Need for careful, continuous observation |
Empirical Antibiotic Therapy
|
Duration Therapy |
||
|
Class 2: mild |
oral |
1-2 weeks |
|
Class 3 / 4: moderate / severe |
oral/initially iv |
2-4 weeks |
Mild infection in an adult
Treat with oral antibiotics; gram-positive cocci (staphylococci and streptococci) are the most common pathogens in acute infection and narrow-spectrum therapy is appropriate.
Flucloxacillin
- Flucloxacillin (0.5 to 1 g orally four times daily)
Or
Clarithromycin
- Clarithromycin (500 mg orally twice daily)
Or
Doxycycline
- Doxycycline (200 mg orally on the first day, followed by 100-200 mg once daily)
Or
Dicloxacillin
Or
Clindamycin
Or
Cefalexin
Or
if MRSA is suspected
Amoxicillin/Clavulanate
Or
Levofloxacin
Or
Doxycycline
Or
Trimethoprim/Sulfamethoxazole.
Treatment is recommended for 7 days, but it may require a further 7 days for a full resolution.
When assessing the need for a longer course of antibiotics for a mild infection, it is important to note that full resolution of skin symptoms is not expected within the first 7 days of treatment.
Further diagnostic tests or alternative treatments may need to be considered if the infection has not resolved after 4 weeks.
Moderate infection in an adult
Oral or intravenous antibiotics are recommended.
Flucloxacillin With Or Without Gentamicin And/Or Metronidazole
- Flucloxacillin : 1 g orally four times daily; 1-2 g intravenously every 6 hours
- Gentamicin: 5-7 mg/kg intravenously every 24 hours
- Metronidazole: 400 mg orally three times daily; 500 mg intravenously every 8 hours
Or
Amoxicillin/Clavulanate With Or Without Gentamicin
- Amoxicillin/clavulanate: 500/125 mg orally three times daily; 1.2 g intravenously every 8 hours Intravenous dose consists of 1 g of amoxicillin plus 0.2 g of clavulanate.
- Gentamicin: 5-7 mg/kg intravenously once daily
Or
Ceftriaxone Plus Metronidazole
- Ceftriaxone: 2 g intravenously every 24 hours
- Metronidazole: 400 mg orally three times daily; 500 mg intravenously every 8 hours
Or
Trimethoprim/Sulfamethoxazole With Or Without Gentamicin And/Or Metronidazole
- Trimethoprim/sulfamethoxazole: 160/800 mg orally twice daily; 160/800 mg intravenously every 12 hours, may increase to 240/1200 mg every 12 hours in severe infections
- Gentamicin: 5-7 mg/kg intravenously every 24 hours
- Metronidazole: 400 mg orally three times daily; 500 mg intravenously every 8 hours
Consider hospital admission if the patient has a moderate infection that is complex or associated with other comorbidities (e.g., severe peripheral arterial disease, renal failure, or immunosuppression).
Severe infection in an adult
Usually treated as an inpatient with parenteral, broad-spectrum, empirical antibiotics. NICE recommends the same treatment as that for moderate infection in adults (see above).
Ensure review of intravenous antibiotics by 48 hours after initiation and consider switching to an oral regimen if possible.
Review microbiology results when available and adjust antibiotic treatment choice as necessary.
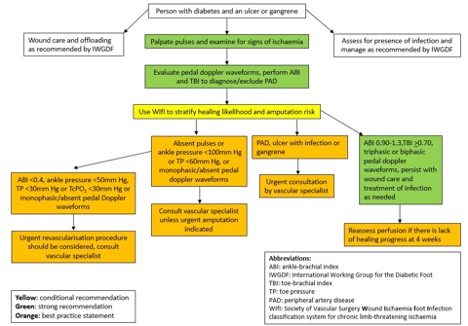
MANAGEMENT OF ISCHEMIA ( PERIPHERAL ARTERY DISEASE (PAD))
- Patients with significant limb ischemia should be referred to a vascular specialist for possible revascularization.
- Revascularization (open, endovascular) should be considered in patients with any degree of limb ischemia and foot ulcer that does not improve over an appropriate time course.
- severe ischemia i.e., an ankle brachial index <0.4, ankle pressure <50mmHg, toe pressure <30mmHg or transcutaneous oxygen pressure <30mmHg or monophasic or absent pedal Doppler waveforms, urgently consult a vascular specialist regarding possible revascularization.
- PAD is less likely in the presence of ABI 0.9-1.3; TBI ≥ 0.70; and triphasic or biphasic pedal Doppler waveforms.
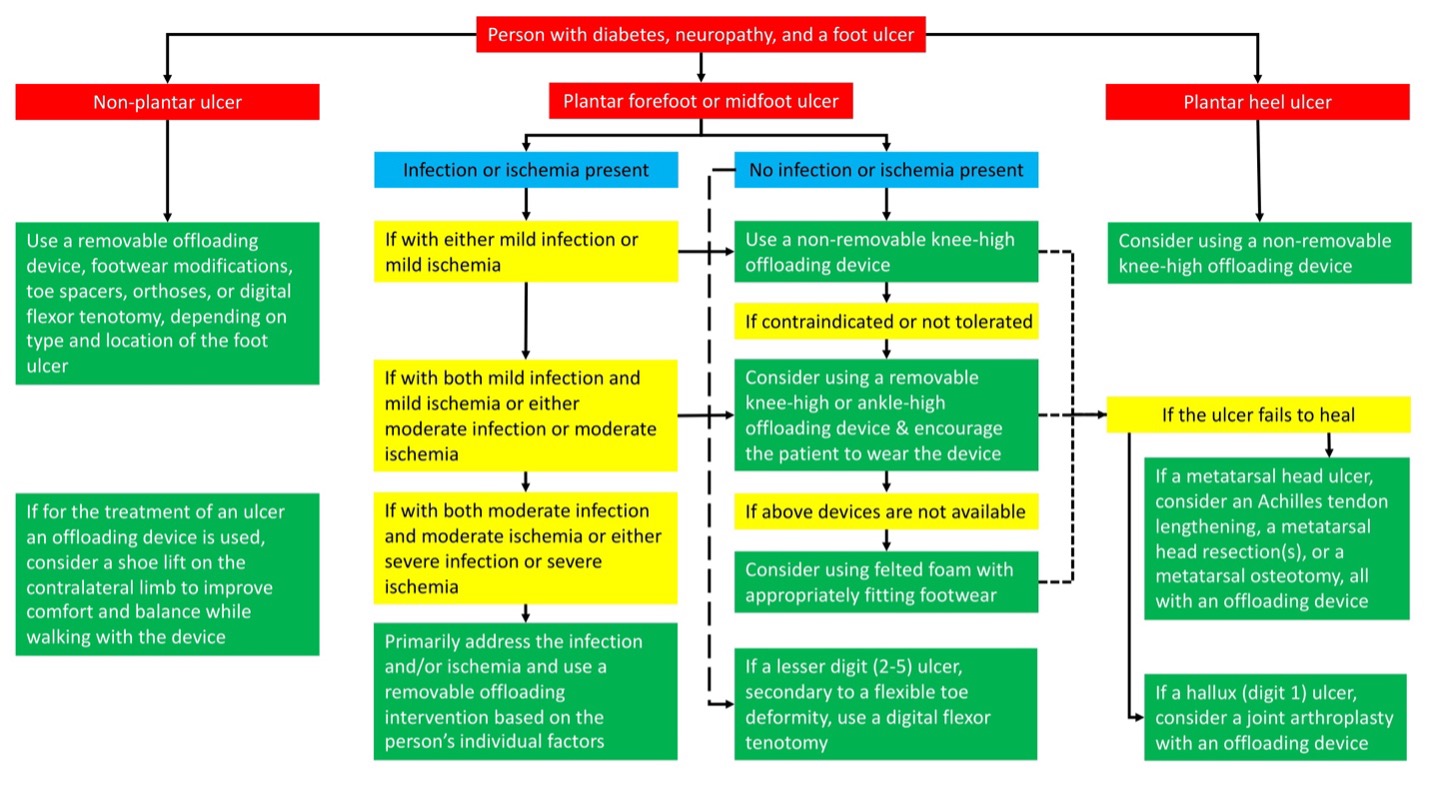
MECHANICAL OFFLOADING
All ulcers subjected to sustained or frequent pressure and stress (ie, pressure-related heel ulcers or medial/lateral foot ulcers) or repetitive moderate pressure (plantar foot ulcers) benefit from pressure reduction, which is accomplished with mechanical offloading.
Offloading devices include :
Total contact cast

-
Cast walkers
An alternative to total contact casting is a prefabricated brace called a cast walker that is designed to maintain a total contact fit. Several cast walkers (nonremovable, removable) are commercially available and provide the capability to offload the foot similar to contact casts.
Therapeutic shoes
After healing of the ulcer is achieved, prescriptive shoes with orthotic inserts are often prescribed to prevent recurrent ulceration.
Knee walkers

Knee walkers are ambulatory assist devices that may be indicated for anyone with a lower extremity issue where weight bearing needs to be avoided. These devices are becoming more popular in the treatment of diabetic ulcer as a means to offload the foot.
WOUND HEALING
Debridement
- When surgeons with expertise in sharp debridement are available, we prefer this method. Sharp debridement, the most widely used method, involves the use of a scalpel or scissors to remove necrotic tissue.
- As an alternative, we suggest application of a hydrogel, but data are limited to support its efficacy in promoting ulcer healing.
- Enzymatic debridement (topical application of proteolytic enzymes such as collagenase) may be more appropriate in certain settings (eg, extensive vascular disease not under team management).
- Autolytic debridement may be a good option in patients with painful ulcers, using a semiocclusive or occlusive dressing to cover the ulcer so that necrotic tissue is digested by enzymes normally present in wound tissue.
Dressings:
After debridement, ulcers should be kept clean and moist but free of excess fluids. Dressings should be selected based upon ulcer characteristics, such as the extent of exudate, desiccation, or necrotic tissue.
|
Ulcer Type |
Type of dressing |
Example |
|
Dry wounds |
Hydrocolloid dressings |
DuoDERM or IntraSite Hydrocolloid |
|
Exudative wounds |
Absorptive dressings |
Calcium Alginates (eg, Kaltostat, Curasorb) |
|
Very exudative wounds |
Impregnated gauze dressings |
Mesalt |
|
Hydrofiber dressings |
Aquacel, Aquacel-Ag |
|
|
Infected wounds |
Silvadene (silver sulfadiazine) |
|
|
Bacitracin-Zinc Or Neosporin Ointment |
||
|
Fragile periwound skin |
Hydrogel sheets and nonadhesive forms |
Adjunctive local therapies:
Negative pressure wound therapy (NPWT)
NPWT, also called vacuum-assisted closure (VAC), involves the application of controlled subatmospheric pressure to the surface of the ulcer. NPWT enhances healing by increasing wound perfusion, reducing edema, reducing the local bacterial burden, and increasing the formation of granulation tissue.
Growth factors
different growth factors predominantly used as topical agents.
Hyperbaric oxygen therapy (HBOT)
Hyperbaric oxygen therapy (HBOT) may be associated with improved healing as a component of diabetic ulcer management, but the indications for HBOT in the treatment of nonhealing diabetic foot ulcers remain uncertain.
Topical oxygen therapy
Topical oxygen therapy/continuous diffusion of oxygen appears to be associated with improved healing of diabetic foot ulcers.
Shock wave therapy
Shock wave therapy, which consists of treatment using a handheld probe to deliver high-energy pulses locally to the wound, purportedly increases local perfusion and angiogenesis, disrupts biofilm, and may upregulate growth factors.
